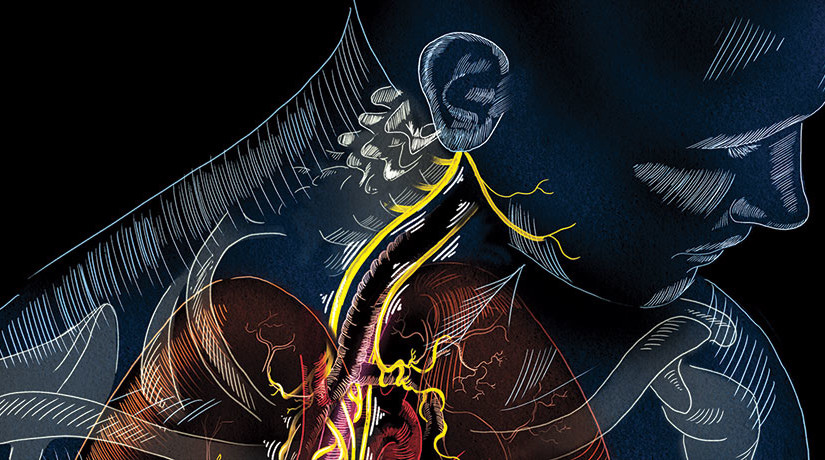
With outposts in nearly every organ and a direct line into the brain stem, the vagus nerve is the nervous system’s superhighway. About 80 percent of its nerve fibers — or four of its five “lanes” — drive information from the body to the brain. Its fifth lane runs in the opposite direction, shuttling signals from the brain throughout the body.
Doctors have long exploited the nerve’s influence on the brain to combat epilepsy and depression. Electrical stimulation of the vagus through a surgically implanted device has already been approved by the U.S. Food and Drug Administration as a therapy for patients who don’t get relief from existing treatments.
Now, researchers are taking a closer look at the nerve to see if stimulating its fibers can improve treatments for rheumatoid arthritis,
SUPER-HIGHWAY The vagus nerve runs from the brain stem down the neck and into the abdomen, reaching a slew of organs in the process.
NICOLE RAGER FULLER
heart failure, diabetes and even intractable hiccups. In one recent study, vagus stimulation made damaged hearts beat more regularly and pump blood more efficiently. Researchers are now testing new tools to replace implants with external zappers that stimulate the nerve through the skin.
But there’s a lot left to learn. While studies continue to explore its broad potential, much about the vagus remains a mystery. In some cases, it’s not yet clear exactly how the nerve exerts its influence. And researchers are still figuring out where and how to best apply electricity.
“The vagus has far-reaching effects,” says electrophysiologist Douglas Zipes of Indiana University in Indianapolis. “We’re only beginning to understand them.”
The wanderer
Anchored in the brain stem, the vagus travels through the neck and into the chest, splitting into the left vagus and the right vagus. Each of these roads is composed of tens of thousands of nerve fibers that branch into the heart, lungs, stomach, pancreas and nearly every other organ in the abdomen. This broad meandering earned the nerve its name — vagus means “wandering” in Latin — and enables its diverse influence.
The nerve plays a role in a vast range of the body’s functions. It controls heart rate and blood pressure as well as digestion, inflammation and immunity. It’s even responsible for sweating and the gag reflex. “The vagus is a huge communicator between the brain and the rest of the body,” says cardiologist Brian Olshansky of the University of Iowa in Iowa City. “There really isn’t any other nerve like that.”
The FDA approved the first surgically implanted vagus nerve stimulator for epilepsy in 1997. Data from 15 years of vagus nerve stimulation in 59 patients at one hospital suggest that the implant is a safe, effective approach for combating epilepsy in some people, researchers in Spain reported in Clinical Neurology and Neurosurgery in October. Twenty of the patients experienced at least 50 percent fewer seizures; two of those had a 90 percent drop in seizures. The most common side effects were hoarseness, neck pain and coughing. In other research, those effects often subsided when stimulation was stopped.
Early on, researchers studying the effects of vagus stimulation on epilepsy noticed that patients experienced a benefit unrelated to seizure reduction: Their moods improved. Subsequent studies in adults without epilepsy found similar effects. In 2005, the FDA approved vagus nerve stimulation to treat drug-resistant depression.
Although many details about how stimulation affects the brain remain unclear, studies suggest that vagus stimulation increases levels of the neurotransmitter norepinephrine, which carries messages between nerve cells in parts of the brain implicated in mood disorders. Some antidepressant drugs work by boosting levels of norepinephrine. Silencing norepinephrine-producing brain cells in rats erased the antidepressant effect of vagus nerve stimulation, scientists reported in the Journal of Psychiatric Research in September.
Against the swell
Vagus stimulation for epilepsy and depression attempts to target the nerve fibers that shuttle information from body to brain. But its fifth lane, which carries signals from brain to body, is a major conductor of messages controlling the body’s involuntary functions, including heart rhythms and gut activity. The nerve’s southbound fibers can also be a valuable target for stimulation.
Around 15 years ago, scientists determined that the brain-to-body lane of the vagus plays a crucial role in controlling inflammation. While testing the effects of an anti-inflammatory drug in rats, neurosurgeon Kevin Tracey and his colleagues found that a tiny amount of the drug in the rats’ brains blocked the production of an inflammatory molecule in the liver and spleen. The researchers began cutting nerves one at a time to find the ones responsible for transmitting the anti-inflammatory signal from brain to body.
“When we cut the vagus nerve, which runs from the brain stem down to the spleen, the effect was gone,” says Tracey, president and CEO of the Feinstein Institute for Medical Research in Manhasset, N.Y. Later research indicated that stimulating undamaged vagus fibers also had anti-inflammatory effects in animals.
Vagus stimulation prompts release of acetylcholine, Tracey and colleagues reported in 2000. Acetylcholine, a neurotransmitter like norepinephrine, can prevent inflammation.
In 2011, rheumatologist Paul-Peter Tak, of the University of Amsterdam, and his colleagues implanted vagus nerve stimulators into four men and four women who had rheumatoid arthritis, an autoimmune inflammatory condition that causes swollen, tender joints. After 42 days of vagus stimulation — one to four minutes per day — six of the eight arthritis patients experienced at least a 20 percent improvement in their pain and swelling. Two of the six had complete remission, the researchers reported at an American College of Rheumatology conference in 2012.
“From a scientific perspective, it’s an extremely exciting result,” says Tak, who is also a senior vice president at GlaxoSmithKline pharmaceuticals based in Stevenage, England. Despite advances in treatments over the last two decades, rheumatoid arthritis patients need better options, he says. In 2014, Tak and his colleagues reported that vagus stimulation reduced inflammation and joint damage in rats with arthritis. After a week of once-daily, minute-long stimulation sessions, swelling in the rats’ ankles shrank by more than 50 percent, the scientists reported in PLOS ONE.
If these results hold up in future studies, Tak hopes to see the procedure tested in a range of other chronic inflammatory illnesses, including inflammatory bowel disorders such as Crohn’s disease. Studies in animals have shown promise in this area: In 2011, researchers reported in Autonomic Neuroscience: Basic and Clinical that vagus stimulation prevented weight loss in rats with inflamed colons.
Treating inflammatory conditions with vagus stimulation is fundamentally different from treating epilepsy or depression, Tak says. More research with patients will be necessary to develop the technique. “We are entering a completely unknown area, because it’s such a new approach,” he says. There could be financial hurdles as well, he says. But GlaxoSmithKline, which Tak joined after initiating the arthritis study, has purchased shares of SetPoint Medical, a company in Valencia, Calif., that produces implantable vagus nerve stimulators, Tak says.
As he and others put stimulation to the test for inflammation, some scientists are attempting to see if manipulating the nerve can help heal the heart.
Taking heart
The vagus nerve has profound control over heart rate and blood pressure. Patients with heart failure, in which the heart fails to pump enough blood through the body, tend to have less active vagus nerves. Trying to correct the problem with electrical stimulation makes sense, says Michael Lauer, director of the cardiovascular sciences division at the National Heart, Lung and Blood Institute in Bethesda, Md. “It’s a great idea.”
Yet so far, results from studies on the effects of vagus stimulation on heart failure have been inconsistent. In 2011, researchers reported in the European Heart Journal that repeated vagus nerve stimulation improved quality of life and the heart’s blood-pumping efficiency in heart failure patients. A vagus stimulation trial of heart failure patients in India published in the Journal of Cardiac Failure in 2014 echoed these results. After six months of therapy, the patients’ left ventricles pumped an average of 4.5 percent more blood per beat.
Last August, however, researchers reported that a six-month clinical trial of vagus stimulation failed to improve heart function in heart failure patients in Europe. This study had the most participants — 87 — but used the lowest average level of electrical stimulation. “All the results thus far are preliminary. The studies that have been finished to date are relatively small,” Lauer says. “But there certainly are promising findings that [suggest] we may be barking up the right tree.”
Another group of scientists is testing more intense vagus stimulation for patients with heart failure. The trial, called INOVATE-HF, is funded by the Israeli medical device company BioControl Medical and uses a higher level of electrical current than the European study that showed no measurable improvements.
“If you try to lower blood pressure and you take a quarter of a pill instead of one pill, blood pressure won’t change,” says cardiologist Peter Schwartz of the IRCCS Istituto Auxologico Italiano in Milan. It’s equally important to use the right dose of vagus stimulation, he says. The new trial is also much larger than earlier studies, with more than 700 patients enrolled internationally. Results are expected by the end of 2016.
Vagus manipulation isn’t limited to heart failure research. It’s also being tried in atrial fibrillation, in which the heart flutters erratically. “When it flutters, it doesn’t really push blood very efficiently,” says clinical electrophysiologist Benjamin Scherlag of the University of Oklahoma in Oklahoma City. Atrial fibrillation is common in people over age 60, Scherlag says, and can ultimately lead to blood clots and strokes. Treatments include drugs that alter heart rhythm or thin the blood, but they don’t work for all patients and some have nasty side effects, Scherlag says.
In the lab, scientists can use high-intensity vagus stimulation to alter heart rhythm and induce atrial fibrillation in animals. But milder stimulation that alters heart rate only slightly, if at all, can actually quell atrial fibrillation, animal studies and one human study show.
Vagus stimulation for atrial fibrillation is still in its infancy, and clinical applications haven’t been adequately tested, says Indiana’s Zipes. “Nevertheless, the concept bears looking into.”
At intensities so low they didn’t cause any perceptible change in heart rate, vagus stimulation controlled atrial fibrillation in dogs, Scherlag and colleagues reported in 2011. In 20 people receiving surgery for atrial fibrillation, low-level vagus stimulation reduced the duration of heart fluttering episodes from an average of 16.7 minutes to an average of 10.4 minutes, Scherlag and his colleagues reported in the Journal of the American College of Cardiology in March.
In their study, Scherlag and his colleagues didn’t implant a nerve stimulator. In fact, they didn’t directly contact the nerve at all. They accessed tendrils of the vagus through the skin of their patients’ ears. Other researchers are also testing devices that stimulate the nerve without surgery.
Skin deep
“Vagal nerve stimulation is very nice, but in order to get to the vagus nerve … you have to cut down surgically,” Scherlag says. “This is not the kind of thing you want to do, except under extreme situations.”
But in the ear, tiny fingers of the vagus’s fibers run close to the surface of the skin, primarily under the small flap of flesh, the tragus, that covers the ear’s opening. Studies have explored using stimulation of those fibers through the skin of the ear to treat heart failure, epilepsy and depression, as well as memory loss, headaches and even diabetes — a reflection of the nerve’s control over a variety of hormones in addition to acetylcholine and norepinephrine.
Stimulating the vagus nerve through the ear of diabetic rats lowered and controlled blood sugar concentrations, researchers from China and Boston reported in PLOS ONE in April. The stimulation prompted the rats’ bodies to release the hormone melatonin, which controls other hormones that regulate blood sugar.
Ear-based vagus stimulation appeared to improve memory slightly in 30 older adults in the Netherlands. After stimulation, study subjects were better able to recall whether they had been shown a particular face before, says study coauthor Heidi Jacobs, a clinical neuroscientist at Maastricht University in the Netherlands. The researchers, who reported the work in the May Neurobiology of Aging, plan to investigate whether these effects last over time and exactly how the stimulation affects the brain, Jacobs says.
The ear isn’t the only nonsurgical target. The company electroCore, based in Basking Ridge, N.J., manufactures a small, handheld device that can stimulate the vagus when placed on the throat. The company initially tested the devices to reduce asthma symptoms — relying on the nerve’s anti-inflammatory action. But during testing, patients reported that their headaches were disappearing, says J.P. Errico, CEO of electroCore. Now, the company is investigating the use of an electroCore device to treat chronic cluster headaches, severe headache attacks that can come and go for over a year. People suffering from an average of 67.3 cluster headaches each month experienced around four fewer attacks per week on average when using the device along with standard treatments like drugs, researchers reported in Cephalalgia in September.
Several researchers have reservations about skin-deep stimulation. “The advantages of the handheld devices are that there’s no surgery required,” says Feinstein Institute’s Tracey, who is a founder and consultant for implant maker SetPoint Medical. But patient compliance becomes an issue. “Patient compliance with anything, whether it’s swallowing a pill or holding a device, is notoriously difficult,” he says.
If a stimulator is implanted, a patient can forget about it, Tak agrees. He and Tracey both predict that implants will soon become smaller and safer.
Beyond the mystery switch
Even for depression and epilepsy, Tak says, researchers still need to figure out the best ways of stimulating the vagus — exactly where to place a device, and how much of a shock to deliver.
The nerve’s multitasking, two-way nature makes it a challenge to fully understand and control. It’s hard to know exactly what you’re zapping when you stimulate the vagus nerve, says physiologist Gareth Ackland of University College London. He compares vagus stimulation to flipping on a light switch in one room of a house and discovering that this endows other rooms in the house with magical powers. “I’m not sure which room it’s going to happen in, I’m not sure for how long and I’m not sure if, after a while, it’s going to work or not,” he says.
The intensity of electrical current, duration of stimulation and each patient’s health status could all affect the results of a vagus stimulation trial, Ackland says. And it’s possible that a widespread effect, such as suppressing inflammation caused by the immune system, could even be harmful to some patients.
Ackland says that he and his colleagues agree that the vagus nerve is important. And he’s not ready to discount vagus stimulation as a potential therapy for conditions such as heart failure. But he warns that there’s a good deal of biology left to understand. “There’s an awful lot of basic science and basic clinical research that is needed before launching into a variety of potential interventions,” he says.
For Tracey, it’s about way more than the vagus. “Nobody should overpromise that the vagus nerve is the secret to everything,” he says. But with a better map of the body’s nerves and their functions, the lessons learned by studying the vagus could inform future therapies that use nerve stimulation, he says. If researchers can understand and manipulate a particular circuit in a nerve that controls a specific molecule — for example, a protein involved in pain or even cell division — they could zero in on crucial targets. “The promise,” he says, “is for tremendous precision.”