We know the menagerie of microbes in the gut has powerful effects on our health. Could some of these same bacteria be making a home in our brains? A poster presented here this week at the annual meeting of the Society for Neuroscience drew attention with high-resolution microscope images of bacteria apparently penetrating and inhabiting the cells of healthy human brains. The work is preliminary, and its authors are careful to note that their tissue samples, collected from cadavers, could have been contaminated. But to many passersby in the exhibit hall, the possibility that bacteria could directly influence processes in the brain—including, perhaps, the course of neurological disease—was exhilarating.
“This is the hit of the week,” said neuroscientist Ronald McGregor of the University of California, Los Angeles, who was not involved in the work. “It’s like a whole new molecular factory [in the brain] with its own needs. … This is mind-blowing.”
The brain is a protected environment, partially walled off from the contents of the bloodstream by a network of cells that surround its blood vessels. Bacteria and viruses that manage to penetrate this blood-brain barrier can cause life-threatening inflammation. Some research has suggested distant microbes—those living in our gut—might affect mood and behavior and even the risk of neurological disease, but by indirect means. For example, a disruption in the balance of gut microbiomes could increase the production of a rogue protein that may cause Parkinson’s disease if it travels up the nerve connecting the gut to the brain.
Talking hoarsely above the din of the exhibit hall on Tuesday evening, neuroanatomist Rosalinda Roberts of The University of Alabama in Birmingham (UAB), told attendees about a tentative finding that, if true, suggests an unexpectedly intimate relationship between microbes and the brain.
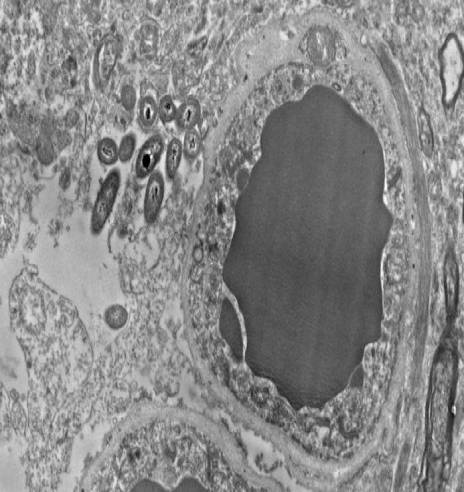
Her lab looks for differences between healthy people and those with schizophrenia by examining slices of brain tissue preserved in the hours after death. About 5 years ago, neuroscientist Courtney Walker, then an undergraduate in Roberts’s lab, became fascinated by unidentified rod-shaped objects that showed up in finely detailed images of these slices, captured with an electron microscope. Roberts had seen the shapes before. “But I just dismissed them, because I was looking for something else,” she says. “I would say ‘Oh, here are those things again.’”
But Walker was persistent, and Roberts started to consult colleagues at UAB. This year, a bacteriologist gave her unexpected news: They were bacteria. Her team has now found bacteria somewhere in every brain they’ve checked—34 in all—about half of them healthy, and half from people with schizophrenia.
Roberts wondered whether bacteria from the gut could have leaked from blood vessels into the brain in the hours between a person’s death and the brain’s removal. So she looked at healthy mouse brains, which were preserved immediately after the mice were killed. More bacteria. Then she looked at the brains of germ-free mice, which are carefully raised to be devoid of microbial life. They were uniformly clean.
RNA sequencing revealed that most of the bacteria were from three phyla common to the gut: Firmicutes, Proteobacteria, and Bacteroidetes. Roberts doesn’t know how these bacteria could have gotten into the brain. They may have crossed from blood vessels, traveling up nerves from the gut, or even come in through the nose. And she can’t say much about whether they’re helpful or harmful. She saw no signs of inflammation to suggest they were causing harm, but hasn’t yet quantified them or systematically compared the schizophrenic and healthy brains. If it turns out that there are major differences, future research could examine how this proposed “brain microbiome” could maintain or threaten the health of the brain.
In the initial survey of the electron micrographs, Roberts’s team observed that resident bacteria had puzzling preferences. They seemed to inhabit star-shaped cells called astrocytes, which interact with and support neurons. In particular, the microbes clustered in and around the ends of astrocytes that encircle blood vessels at the blood-brain barrier. They also appeared to be more abundant around the long projections of neurons that are sheathed in the fatty substance called myelin. Roberts can’t explain those preferences but wonders whether the bacteria are attracted to fat and sugar in these brain cells.
Why haven’t more researchers seen bacteria in the brain? One reason could be that few researchers subject postmortem brains to electron microscopy, Roberts says. “Pairing up a neuroanatomist with a brain collection just doesn’t happen very often.” And neuroscientists may—as she did until recently—disregard or fail to recognize bacteria in their samples.
Roberts acknowledges that her team still needs to rule out contamination. For example, could microbes from the air or from surgical instruments make it into the tissue during brain extraction? She plans to hunt for such evidence. She also wants to rule out that the solutions that preserve mouse brains introduce or nourish bacteria. Among visitors to the poster, “There were a few skeptics,” Roberts notes. “I have that part of me, too.” But even if the bacteria were never really thriving in living brains, the patterns of their postmortem invasion are intriguing, she says.
If we really have the brain microbiome Roberts proposes, “There is much to investigate,” says Teodor Postolache, a psychiatrist at the University of Maryland in Baltimore. He has studied the protozoan parasite Toxoplasma gondii, which invades the brain but doesn’t always cause obvious disease. “I’m not very surprised that other things can live in the brain, but of course, it’s revolutionary if it’s so,” he says. If these common gut bacteria are a routine, benign presence in and around brain cells, he says, they might play a key role in regulating the brain’s immune activity. “It’s a long road to actually prove that,” he says, but “it’s an exciting path.”